If's Health Insurance Advantages
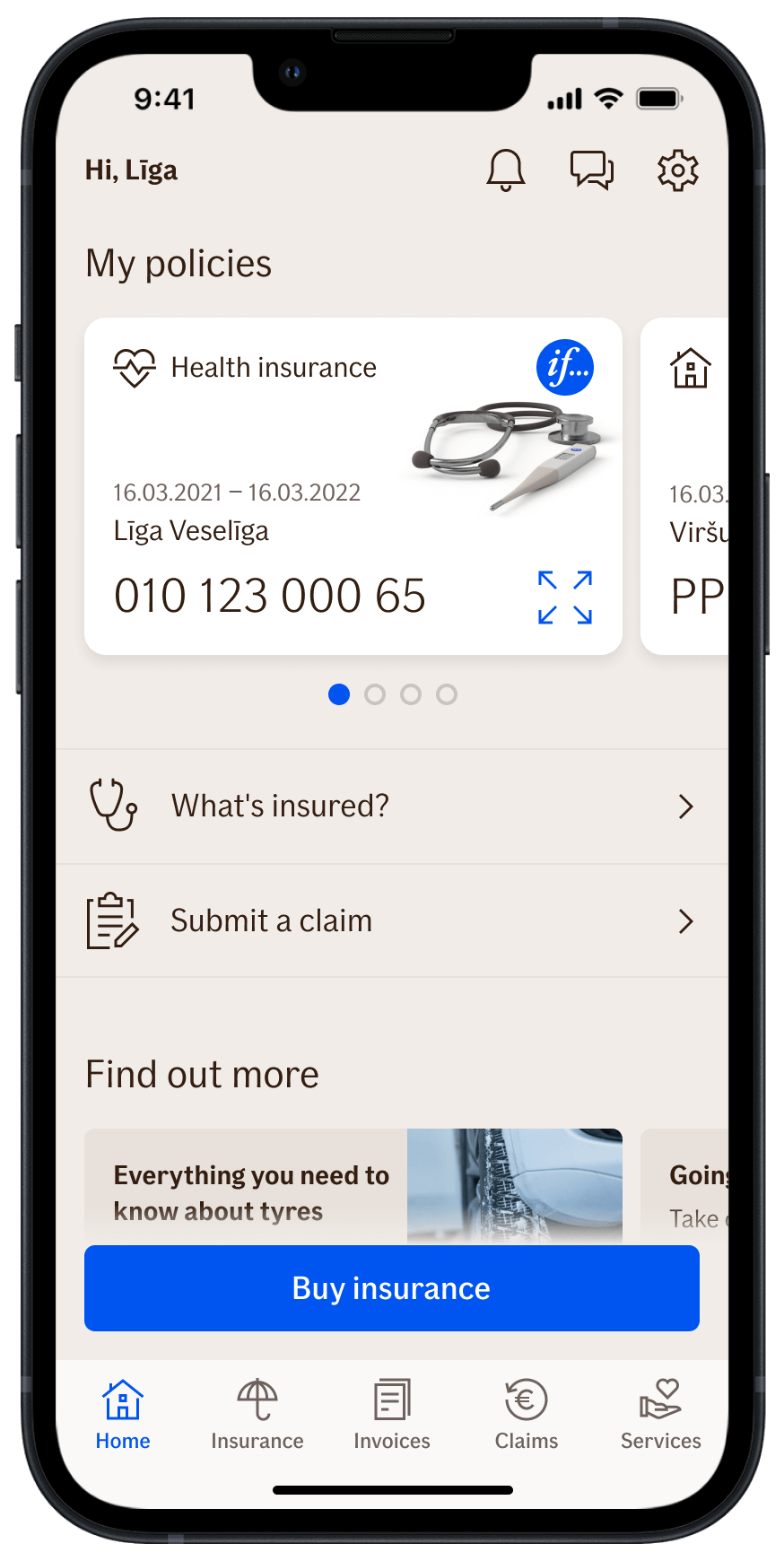
If Mobile Baltics application
A convenient and secure way to manage your health insurance on your smartphone.
e-Doktor
No queueing to see a doctor and get a remote consultation from a family doctor paid for in full by the If health policy.
Broadest range of medical services
No hidden restrictions, exclusions are clearly described. Treatments of previously diagnosed and oncological diseases are also covered.
What does the policy cover
 Covered
Covered
The costs of paid consultations of family physicians or medical specialists without the referral of your family physician, including remote (digital) and home visits. The costs of emergency medical care, special medical transport or disabled person transport. We indemnify the medically indicated procedures, laboratory analyses, diagnostics or high-technology instrumental diagnostics, pregnancy monitoring, day care treatment prescribed by the doctor. Outpatient treatment coverage also includes e-Doctor telemedicine service.
 Not covered
Not covered
The costs of homeopathy treatment, psychologist or psychiatrist, food and nutrition specialist, narcologist, speech therapist, trichologist, sleep studies (sleep disorders and apnea), sexual pathologist or immunotherapy; costs of infertility diagnosis and treatment, sterilization, vasectomy and artificial insemination; medical expenses for any mental illness, addiction, drug addiction, alcoholism, venereal diseases, AIDS and HIV; costs of alternative and/or complementary medical services (e.g. Ayurveda, aromatherapy, etc.); costs of cosmetic and beauty services; costs of whole body magnetic resonance imaging (MRI), positron emission tomography, capsule endoscopic gene analyses, genetic analyses, except genetic analyzes related to pregnancy monitoring, cost of food intolerance tests.
 Consider
Consider
To apply a claim it is also necessary to add a referral for analyses, tests and examinations prescribed by the doctor. As a deviation from the p 3.2.1.2 of the „Terms and Conditions of Health Insurance THE-20251“, consultation and visit fees of psychologists, psychiatrists, psychotherapists, and mental health nurses, as well as tests and examinations related to treatment, are covered under the „Outpatient treatment” Insurance Coverage limit.
 Covered
Covered
The costs of preventive medicine doctor consultation, medical examinations and issuance of medical certificates required for driver’s license, firearm license, food handler’s certificate, etc., medical examinations without a doctor’s referral: health check-up packages (including doctor consultation), full body health check-ups, laboratory analysis packages, sports medicine specialist consultations, sports examinations and stress tests, comprehensive allergen (panel) test, antibody tests, food intolerance tests, genetic tests, sexually transmitted disease tests.
 Not covered
Not covered
The costs of tests intended for home use.
 Consider
Consider
The costs are covered if the services are conducted at the facilities of a medical institution or pharmacy. As a deviation from the p 3.2.3.1 of the „Terms and Conditions of Health Insurance THE-20251”, genetic tests and tests for sexually transmitted diseases are not covered under the „Preventive medical examinations” Insurance Coverage. As a deviation from the p 3.2.3.1 of the „Terms and Conditions of Health Insurance THE-20251”, comprehensive eye examinations are covered under the „ Preventive medical examinations ” Insurance Coverage limit.
 Covered
Covered
The costs of rehabilitation consultations, doctor-prescribed: physiotherapy (including kinesitherapy, shockwave therapy, magnet therapy, electrotherapy, chiropractic treatment, osteopathy, ultrasound therapy, inhalation therapy, light therapy, hydrotherapy, salt therapy in a salt chamber, paraffin therapy, mud therapy, electromagnetic muscle stimulation (EMLS), occupational therapy, etc.), therapeutic massage as manual therapy, classical and sports massage, as well as lymphatic massage related to treatment, therapeutic exercise (including therapeutic swimming, water exercise, etc.), speech therapy (logopedic therapy) and myofunctional therapy, medical or orthopedic aids used for trauma or rehabilitation purposes (including orthoses, crutches, wheelchairs, orthopedic shoes, insoles, support belts, prostheses, etc.).
 Not covered
Not covered
The costs of the following services and aids: sports to strengthen or maintain general health, general massage, lymphatic massage, vacuum massage, cryomassage, for beauty or wellness services, services not mentioned in the previous point and related medicines and aids. The costs for compression socks or stockings intended for vein treatment or sclerotherapy (such costs are indemnified under Vein treatment and sclerotherapy).
 Consider
Consider
The costs are covered if the provider of rehabilitation services (except for swimming pools) holds an activity licence or a professional certificate to provide of the relevant outpatient medical rehabilitation service. A doctor’s referral must be attached to the claim application.
 Covered
Covered
The costs of medically indicated inpatient services, provided that the Insured Person stays overnight in the hospital: consultations, diagnostic examinations, surgical treatment (all types of surgery using the latest technologies, including spinal, neuro-surgical, micro-surgical, laparoscopic, cardiovascular, arthroscopic, etc.), intensive care, planned and emergency surgeries (including those related to oncological diseases), costs of medicines and medical aids prescribed and used in the hospital, daily hospital bed fee, and private ward service.
 Not covered
Not covered
The costs of obstetrical expenses, cosmetic surgery, plastic surgery, vision correction, stomach reduction surgery, diastasis surgery, surgery related to infertility and tubal patency surgeries, vein surgery, sclerotherapy, gender reassignment surgeries, rehabilitatiion services in hopital, childbirth and maternity care services, as well as gratitude payments or gifts to the doctor as a token of appreciation.
 Consider
Consider
The hospital treatments must be previously agreed with If. As a deviation from the p 3.2.6.3 of the „Terms and Conditions of Health Insurance THE-20251“, the costs of a paid ward and hospital meals related to childbirth for the insured person or when insured person is the father of the child, are reimbursed under the „Hospital treatment“ Inusrance coverage limit. This special clause does not apply to other childbirth-related costs.
 Covered
Covered
The costs of f the vaccine, the vaccination fee, and the vaccination certificate fee.
 Consider
Consider
The costs are covered if the vaccination is conducted at the facilities of a medical institution or pharmacy. The cost of a consultation related to vaccination is covered under the “Outpatient Treatment” Insurance Coverage.
 Covered
Covered
The costs for medicines prescribed by the doctor, which are registered in the European Union Medicines Register.
 Not covered
Not covered
The costs of medicines prescribed for the treatment of health disorders caused by the consumption of tobacco products, alcohol, narcotics, or other psychoactive substances, weight-loss medicines; medicines affecting fertility or potency, vaccines, mechanical aids for sleep, e.g. CPAP mask, etc., diagnostic products, such as thermometers, infusion pumps, inhalers, over-the-counter self-tests for home use, disposable containers for samples, medical or orthopedic aids used for trauma treatment or rehabilitation (including orthoses, crutches, wheelchairs, orthopedic shoes, insoles, support belts, prostheses, etc.).
 Consider
Consider
The original or a copy of the doctor’s prescription must be attached to the claim application. As a deviation from the p 3.2.8.1 of the „Terms and Conditions of Health Insurance THE-20251”, prescription drugs related to mental health (including, for example, antidepressants, stimulants, sleeping pills, and sedatives) are not covered under the „Prescription Medicines” Insurance Coverage.
 Covered
Covered
The costs of oral hygiene services (including soda cleaning, pearl cleaning, tartar removal, etc.), consultations and dental treatment, including caries treatment, root canal treatment, periodontology, orthodontics, prosthetics, crowns, dental implants (including porcelain), aftercare of prostheses, crowns, and implants, tooth restoration using laboratory-made ceramic or metal fillings (e.g., inlay, onlay, or overlay), placement of veneers and aligners, injections required for treatment, X-rays, tooth extraction, and anesthesia, oral surgery (surgical treatment of teeth and jaw/jawbone diseases and all related services).
 Not covered
Not covered
The costs of teeth whitening and other aesthetic dental services, medications prescribed by a doctor (e.g., painkillers, antibiotics, etc. after tooth extraction), expenses for hygiene, care, and beauty products (e.g., toothpaste, dental floss, toothbrush, mouthwash, dental decorations, etc.).
 Covered
Covered
The costs of purchase of glasses or contact lenses prescribed by a doctor or optometrist, repair of glasses or replacement of lenses.
 Not covered
Not covered
The costs of purchase of non-prescription glasses, including blue-light blocking glasses for preventive protection when working with computers, and sunglasses, colored non-optical glasses or lenses, purchase of care products and accessories for glasses or lenses, e.g., glasses cases, lens containers, cleaning cloths, storage or cleaning solutions, etc., medications (including eye drops, etc.), vitamins, and dietary supplements.
 Consider
Consider
The costs of purchasing glasses or contact lenses are reimbursed only if the purchase is made in a registered optical store or pharmacy in Estonia, Latvia, or Lithuania.
 Covered
Covered
The costs of vein surgery, including leg vein operations, and related hospital care, sclerotherapy, compression stockings or socks prescribed by a doctor.
 Consider
Consider
The vein surgery must be previously agreed with If. As a deviation from the p 3.2.14.1 of the „Terms and Conditions of Health Insurance THE-20251“, visit and consultation fees related to vein treatment, as well as the costs of physician-indicated analyses and procedures, are covered under the „Vein Treatment” Insurance Coverage limit. Procedures carried out for aesthetic purposes are not covered.
 Covered
Covered
In the event of critical illnesses, the insurance company will pay out compensation in the amount of the sum insured in conformity with critical illness insurance terms and conditions TCI_EE_20251.. Critical illnesses – myocardial infarction (heart attack), stroke, malignant tumor (cancer), heart valve insufficiency requiring surgery for valve replacement or function restoration, chronic kidney failure, multiple sclerosis, organ transplantation, blindness, deafness, loss of speech, limb paralysis or loss, benign brain tumor, third-degree and higher burns, type 1 diabetes mellitus (primary), aplastic anemia, amyotrophic lateral sclerosis (ALS), aortic aneurysm with surgical treatment, coronary heart disease with surgical treatment, cerebral aneurysm with surgical treatment, idiopathic Parkinson’s disease (up to age 65), Alzheimer’s disease (up to age 65).
Terms
- Insurance provider - If P&C Insurance AS
-
Please study the documents regulating health insurance in the Insurance Company's website www.if.ee in the Health Insurance section Terms and conditions:
- Health Insurance Conditions
- General Insurance Conditions
- Health Insurance Product Information Page
- The content and exclusions of the insurance cover are specified in the insurance terms and conditions
- Handling personal data: https://www.if.ee/isikuandmed
